
Navigating Post-Operative Mental Health: The Journey to Emotional Wellness
- When we prepare for surgery, our focus is almost entirely on the physical aspect of the “cure.” We research the surgeon’s success rates, prepare our homes for physical limitations, and stock up on bandages. However, the impact on post-operative mental health is often an afterthought. Many patients are surprised to find that while their physical wounds are healing, they are struggling with unexpected feelings of sadness, anxiety, or frustration.
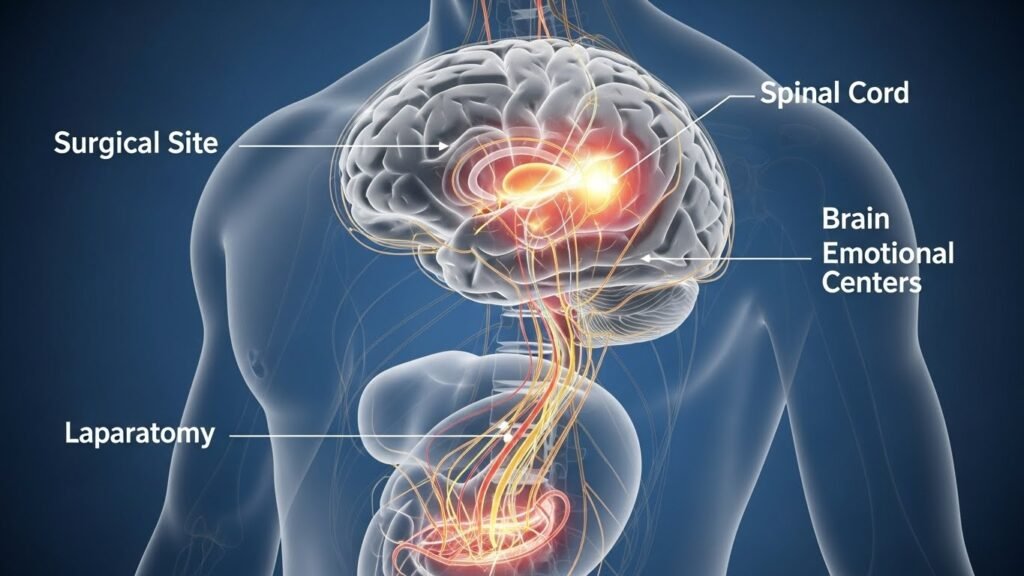
The truth is that surgery is a significant event for the brain and the nervous system, not just the body. The combination of anesthesia, physiological stress, and the sudden loss of independence can create an emotional “slump” that is a very real part of the healing process. Addressing your mental well-being is just as critical as managing your physical pain. In this guide, we will explore why these emotional shifts happen and how you can manage your mental health during the “care” phase of recovery.
The Science of the “Post-Surgery Blues”
It is estimated that a significant percentage of patients experience some form of low mood or “blues” following a procedure. Several biological factors contribute to this state:
- Anesthesia After-Effects: General anesthesia can affect brain chemistry for several days or even weeks, leading to “brain fog” and emotional instability.
- The Inflammatory Response: Surgery triggers systemic inflammation. Research shows a strong link between high inflammation levels and symptoms of depression.
- Sleep Disruption: Between hospital noises and physical discomfort, sleep quality usually plummets after surgery. Sleep deprivation is a primary driver of irritability and anxiety.
Everyday Emotional Experiences After Surgery
Understanding that your feelings are a physiological response can help remove the stigma. You are not “being difficult”; your body is processing trauma.
1. Frustration and Loss of Control Going from a fully independent adult to someone who needs help with basic tasks like bathing or dressing can be demoralizing. This loss of agency often manifests as anger or a “short fuse” with caregivers.
2. Post-Surgical Anxiety. It is common to feel hyper-vigilant about your body. Every twinge of pain or itch at the incision site can trigger a fear that something is going wrong. This “health anxiety” can make it difficult to relax and focus on recovery.
3. The “Post-Op Slump” Often occurring 3 to 5 days after returning home, this is a period of profound fatigue and sadness. The initial adrenaline of getting through the surgery wears off, and the reality of the long road to recovery sets in.
Strategies for Managing Post-Operative Mental Health
The key to maintaining your mental health is treating it with the same discipline you use for your physical health.
Establish a “Micro-Routine.” When you are bedbound, days can bleed into each other. Creating a small routine helps provide a sense of normalcy. Try to wake up, wash your face, and change out of your pajamas at the same time every day. These small acts of self-care signal to your brain that you are still in control.
Practice “Box Breathing.” Anxiety triggers the “fight or flight” response. You can manually override this by using box breathing: inhale for 4 seconds, hold for 4, exhale for 4, and hold for 4. This simple technique lowers your heart rate and grounds you in the present moment.
Limit Information Overload. While being an advocate is good, “doom-scrolling” through medical forums at 2:00 AM is not. If you have concerns about your post-operative mental health or physical progress, write them down for your doctor rather than searching for worst-case scenarios online.

The Role of Nutrition in Mood
The “gut-brain axis” means that the foods we discussed for wound healing also play a role in mental wellness.
- Omega-3s: Found in salmon and walnuts, these are essential for brain health and can help mitigate depressive symptoms.
- Magnesium: Found in leafy greens and dark chocolate, it acts as a natural relaxant for the nervous system.
- Hydration: Even mild dehydration can lead to confusion and increased irritability.
When Is It More Than Just the “Blues”?
While a temporary slump is typical, it is essential to recognize when post-operative mental health issues require professional intervention. Post-operative depression or PTSD (Post-Traumatic Stress Disorder) can occur, especially after emergency or life-threatening procedures.
Contact your healthcare provider if you experience:
- Feelings of hopelessness lasting longer than 2 weeks.
- Thoughts of self-harm or that your family would be better off without you.
- Panic attacks that prevent you from eating or sleeping.
- Complete social withdrawal and refusal to speak with loved ones.

How Caregivers Can Help
If you are providing “care” for someone after surgery, your role in their mental health is vital.
- Validate, Don’t Dismiss: Avoid saying “at least the surgery was a success.” Instead, say “Understandably, you feel frustrated right now; it’s a lot to handle.”
- Encourage Small Wins: Celebrate when they walk to the kitchen or manage a longer nap.
- Monitor Medications: Some pain medications can cause mood swings or hallucinations. Keep a log of any behavioral changes that appear to be linked to medication timing.

Common Mistakes to Avoid
- Comparing Your Journey: Every person heals at a different rate. Comparing your recovery to a friend’s can lead to unnecessary feelings of failure.
- Rushing Back to Work: Mental energy is a finite resource. Returning to high-stress work before your brain has recovered from the trauma of surgery can lead to burnout and physical setbacks.
- Ignoring the Need for Sunlight: Being stuck in a dark room can disrupt your Vitamin D levels and your mood. Even 10 minutes by a sunny window can make a difference.
The Importance of Social Connection
Isolation is a significant risk factor for poor post-operative mental health. While you might not feel up for a party, small social interactions are healing. A short video call, a neighbor dropping by for ten minutes, or even interacting with a pet can release oxytocin, the “bonding hormone” that reduces stress.

Preparing Mentally Before the “Cure”
If your surgery is scheduled in advance, you can “pre-habilitate” your mind.
- Set Realistic Expectations: Ask your surgeon exactly what the first week will look like.
- Build Your Support Team: Know who you can call when you need to vent.
- Plan Your Entertainment: Queue up lighthearted movies or podcasts that make you laugh, as laughter releases endorphins.

Conclusion: Healing the Whole Person
A full recovery is a victory of both the body and the mind. By acknowledging that post-operative mental health is a legitimate part of the process, you remove the power of fear and frustration. Be patient with yourself. Give your mind the same “care” and time you give your physical incision.
The “cure” may happen in the operating room, but the actual healing occurs in the quiet moments of recovery at home. With the right tools, support, and mindset, you will emerge from your surgery not only physically repaired but also emotionally resilient.




