
Mastering Patient Advocacy: How to Effectively Communicate with Your Medical Team
- Navigating the modern healthcare system can be overwhelming. Between short appointment times, complex medical jargon, and the stress of illness, many patients leave their doctor’s office feeling unheard or confused. This is where the concept of patient advocacy becomes essential. Being an advocate means taking an active role in your healthcare decisions, asking the right questions, and ensuring that your “care” plan aligns with your personal values and goals.
Whether you are managing a chronic condition or seeking a “cure” for a sudden illness, you are the most essential member of your medical team. You know your body better than anyone else. By learning the skills of patient advocacy, you can transform a passive medical experience into a collaborative partnership that leads to better health outcomes.
What is Patient Advocacy?
At its core, advocacy is the act of supporting a cause or a person. In a medical setting, it involves ensuring that a patient’s rights are respected and their needs are met. You can be an advocate for yourself or for a family member who may be unable to speak for themselves.
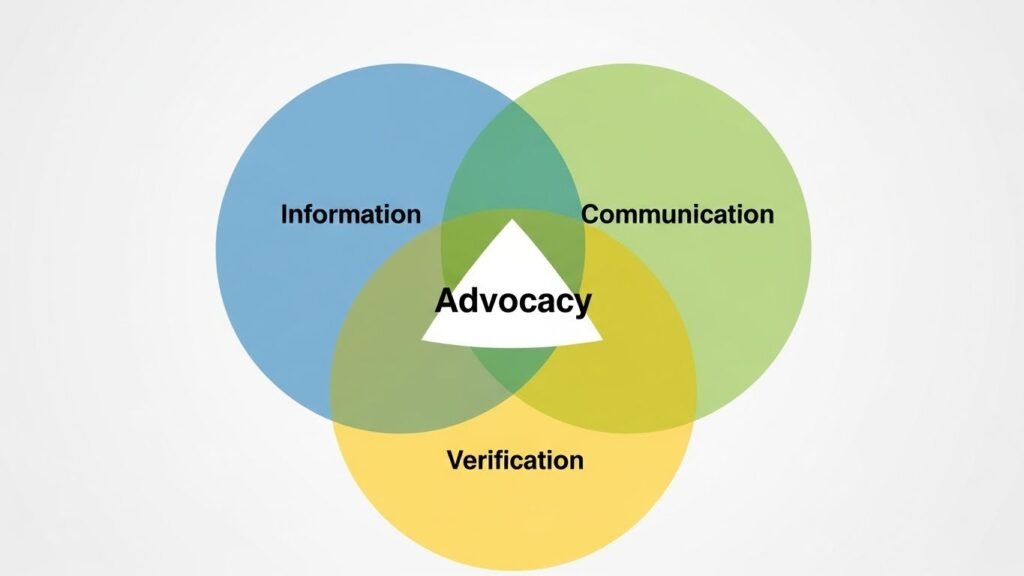
A good advocate focuses on three main pillars:
- Information: Gathering all the facts about a diagnosis and treatment options.
- Communication: Clearly expressing concerns and preferences to the medical staff.
- Verification: Ensuring that the agreed-upon plan is being followed and understood by everyone involved.
Preparing for Your Appointment
Effective patient advocacy begins long before you enter the examination room. Because doctors often have limited time, being prepared ensures that you make the most of every minute.
- The “Top Three” Rule: Identify the three most important questions or concerns you want to address. Write them down and bring them with you.
- Track Your Symptoms: Keep a brief log of when symptoms occur, how long they last, and what triggers them. This data is more helpful to a doctor than a vague memory.
- Update Your Med List: Bring a complete list of all medications, including vitamins and herbal supplements, as these can interact with prescribed treatments.
How to Speak So Your Doctor Will Listen
Communicating with medical professionals is a skill that can be practiced. The goal is to be assertive without being aggressive. Use “I” statements to describe your experience. For example, instead of saying, “You aren’t listening to me,” try, “I feel concerned that we haven’t addressed my fatigue yet.”
Don’t be afraid to ask for clarification. If a doctor uses a term you don’t understand, stop them and say, “Could you explain that in plain English?” A crucial part of patient advocacy is ensuring you have a clear understanding of your own health.

The Power of the “Teachable Back” Method
One of the most effective ways to ensure communication is successful is the “teach-back” method. At the end of the consultation, summarize what you heard in your own words.
You might say: “So, to make sure I have this right, you want me to take this new medication once a day in the morning, and I should see an improvement in a week. If I get a rash, I should call your office immediately. Is that correct?” This gives the doctor a chance to correct any misunderstandings on the spot.
Bringing a Support Person
Sometimes, the best form of patient advocacy is having a second set of ears. Bringing a trusted friend or family member to an appointment can be incredibly helpful. They can take notes, provide emotional support, and remember details you might miss under stress.
If you bring someone, decide beforehand what their role will be. Do you want them to listen, or do you want them to prompt you if you forget to mention a specific symptom?

Seeking a Second Opinion
A common misconception is that asking for a second opinion is disrespectful to your doctor. In reality, second opinions are a standard and respected part of the “cure and care” process, especially for major surgeries or life-altering diagnoses.
A confident doctor will welcome a second opinion because it ensures the patient feels confident about their path forward. When seeking a second opinion, ask for your medical records to be transferred so the new consultant has all the necessary data to provide an informed perspective.
Navigating Disagreements
What happens if you disagree with a recommended treatment? As an advocate, you have the right to refuse a treatment or ask for alternatives. Ask your doctor about the “Risk vs. Benefit” ratio.
- “What happens if we wait a month before starting this?”
- “What are the non-surgical options for this condition?”
- “How will this treatment affect my quality of life daily?”

The Role of Professional Patient Advocates
In complex cases involving multiple specialists, insurance disputes, or long-term hospital stays, consider hiring a professional patient advocate. These are often former nurses or social workers who understand the “ins and outs” of the system and can fight for your rights when you are too tired to do so yourself.
Common Mistakes in Patient Advocacy
- Withholding Information: Some patients feel embarrassed about certain lifestyle habits or symptoms. However, doctors need the whole picture to provide a proper cure.
- Leaving Without a Plan: Never leave an office without knowing exactly what the next step is. Is it a blood test? A follow-up? A new prescription?
- Ignoring Your Intuition: If something feels “off” about a diagnosis, don’t ignore that feeling. Use it as a prompt to ask more questions or seek further testing.

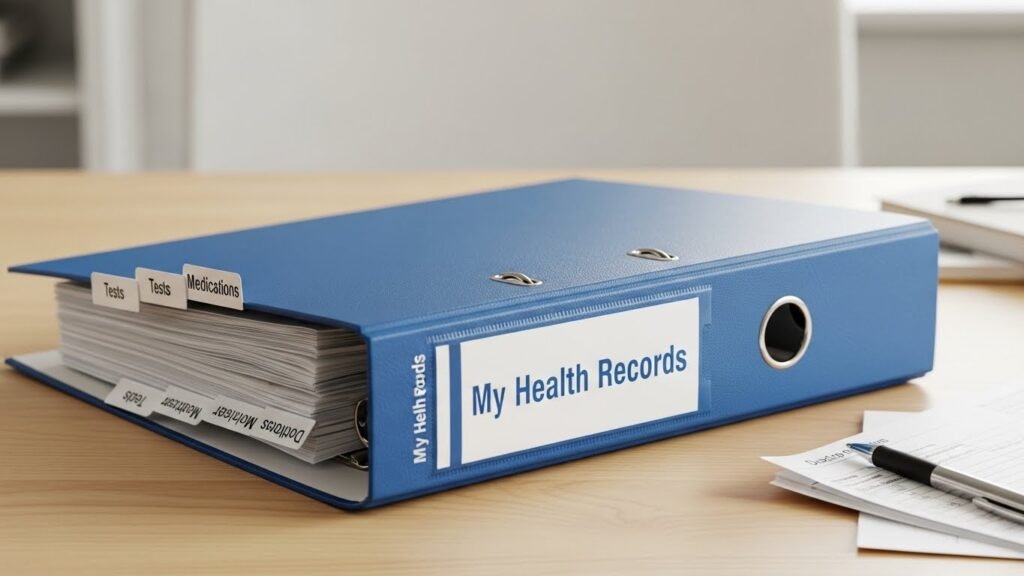
Keeping Your Own Medical Records
In a digital world, medical records are often scattered across different hospital portals. A key part of patient advocacy is maintaining your own “Health Binder.”
Your Health Binder should include:
- Summaries of recent hospital visits.
- Results of imaging (X-rays, MRIs) and blood work.
- A timeline of significant health events.
- Insurance information and contact details for all your specialists.
Having this information ready can save vital time during emergencies and ensure that new doctors have a complete history of your care.
Understanding Your Rights
Most countries have a “Patient Bill of Rights.” These generally include the rights to privacy, informed consent, and respectful care. Knowing these rights empowers you to stand your ground if you feel you are being mistreated or if your privacy is being compromised.
Conclusion
Patient advocacy is not about being a “difficult” patient; it is about being an engaged and informed one. When you speak up, ask questions, and prepare for your appointments, you help your medical team provide better care. The transition from “cure” to “care” is most successful when the patient is at the center of the conversation.
Start small. At your next appointment, ask one extra question or bring a written list. Over time, you will find that your voice is one of the most powerful tools in your medical arsenal. You deserve to be an active participant in your journey toward health.

Advocacy Quick-Start Guide
- Please write it down: Never rely on memory alone.
- Ask “Why?”: Understand the reasoning behind every test or pill.
- Bring a buddy: Two sets of ears are better than one.
- Get the summary: Always ask for a written discharge or visit summary.




